More than half of care providers felt pressured to take in hospital patients who hadn’t been tested for coronavirus (Covid-19) during the height of the pandemic, according to an investigation.
BBC Panorama found that 71 of 124 care providers in England felt pressured by hospitals and councils to receive untested patients as efforts were made to rapidly free up beds.
The findings
Three-quarters (92) of the care providers felt GPs and medical staff were reluctant to visit care homes during March and April, while 73 providers said they felt pressure not to send residents to hospital.
The providers surveyed between 26 June and 14 July are members of Care England or the National Care Home Association and look after more than 350 care homes across the country.
Responses from 39 NHS trusts in England to a Freedom of Information request sent by the programme revealed just one in four patients were tested before being discharged to care homes between 1 March and 15 April.
The programme, BBC Panorama: The Forgotten Frontline, will explore the findings on BBC One at 9pm on 30 July.
“Reckless” and “appalling”
NHS trusts were urged to rapidly discharge hospital patients to free up beds for a predicted surge in need due to coronavirus on 17 March.
But it was not until 15 April that the government said patients should be tested before discharge. A recent Commons report by the cross-party Public Accounts Committee said this was a “reckless” and “appalling” policy error.
The Department of Health and Social Care said its support had ensured that the proportion of coronavirus deaths in care homes is lower in England than many other European countries. A spokesperson said:
It is completely wrong to suggest care homes were an afterthought, and it is an affront to the countless people who have been working to protect care homes since the start of this pandemic.
It is disappointing that BBC Panorama appears to have arrived at its conclusions before considering the evidence.
Throughout the pandemic we have been working closely with the sector and public health experts to put in place guidance and support for adult social care.
“Transferring risk to a poorly supported social care system”
Meanwhile, separate analysis said multiple factors could be behind care home outbreaks, but that rapid discharges “may have played a role in transferring risk to a poorly supported social care system lacking the right protection”.
The Health Foundation said discharges to care homes between 17 March and 30 April were below average, likely due to hospital admissions being down. It suggested the focus of policy action on care homes risked leaving out other groups, such as people receiving care in their own homes.
Deaths from all causes between 23 March and 19 June 2020 of people being cared for at home were 125% higher than the average number across the same period in 2017-19, the organisation noted. This is a bigger proportional increase than the 108% rise in deaths in care homes over the same period.
It’s unclear how many of these additional deaths are due to the indirect impacts of the pandemic or as a result of undiagnosed cases, and the Health Foundation added that more data is needed.
20,000 care home resident deaths
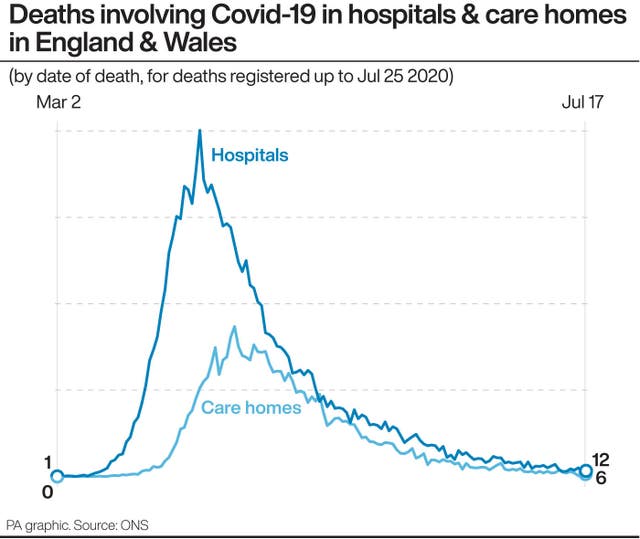
Almost 20,000 care home residents in England and Wales have died with coronavirus, the majority dying in their care home, according to the Office for National Statistics.
Latest figures show deaths from all causes within private homes remain above what would be expected for this time of year. Meanwhile, deaths in care homes, hospitals and other settings have fallen below the five-year average.
The Health Foundation report said:
If these deaths are linked to Covid-19 infection, but not recorded as such, then it raises questions about the adequacy of Covid-19 testing programmes in social care.
It also means that the spread of infection among those receiving social care in the community has been underestimated.
If the deaths have been correctly coded, and are linked to indirect effects of the pandemic (such as delayed access to health or care services), then this would mean that urgent action is needed to address this unmet need.
It comes as county councils warned against a knee-jerk reform of social care that would see the system centralised.
“A centralised system that coronavirus has shown contains huge drawbacks”
It is a year since Boris Johnson promised to “fix” social care during his first speech on the steps of Downing Street, and problems with the fragmented sector have been laid bare by the outbreak.
Members of the County Councils Network say they have strong links to their communities, providers, and other linked council services such as housing and public health which will be lost if care is centrally controlled.
Councillor David Fothergill, spokesperson for health and social care, said:
The harrowing scenes that we have witnessed in our care sector deserve scrutiny, but we should be wary of a knee-jerk reaction that removes democratic oversight from adult social care and places it in a centralised system that coronavirus has shown contains huge drawbacks.

















