A year fighting coronavirus (Covid-19) has left medical staff “burned out”, “fatigued” and “desperately sad”, according to one nurse.
Since the first death in the UK a year ago on Saturday, many doctors, nurses and other frontline workers have been immersed in the battle against Covid-19.
Joanne Morrell, an intensive care nurse at the Calderdale and Huddersfield NHS Foundation Trust, said she would not have believed back in March when she first started working with Covid patients that she and her colleagues would still be dealing with the pandemic nearly a year later.

Disbelief
“We’ve got through it but I just don’t know how we have,” she said.
“I’m in disbelief really that it’s still continuing because I recall, when we got our first (Covid patients) back in March, thinking this will be a few weeks, it’ll all be over and done with, storm in a teacup.
“Then as it continued, I thought by the end of the summer, definitely done… by Christmas time, absolutely gone.
“And here we are, the year later, in the January, and still doesn’t seem to be any closer to this ending any time soon.”
Morrell, 47, said that the hardest aspect of working during the pandemic has been witnessing “the people that are dying unnecessarily”.
She said: “I can deal with stress, I can deal with busy – I’ve worked in A&E and I’ve worked in really busy areas, oncology and assessment units – but it’s the sadness.
“We’re all burned out, we’re all fatigued, but we are also desperately sad.”
https://twitter.com/bumblebee2907/status/1283000871887003648
She added:
When we had the highest death rate, and in one day more people died in this country than in the whole of the pandemic in Australia, that actually broke my heart.
How’s it got to this point? How have we got to over 100,000 people dead? How?”
A steep learning curve
The last year has been a steep learning curve for healthcare professionals, not just in terms of Covid-19 itself but also in establishing new working processes and dealing with unexpected issues.
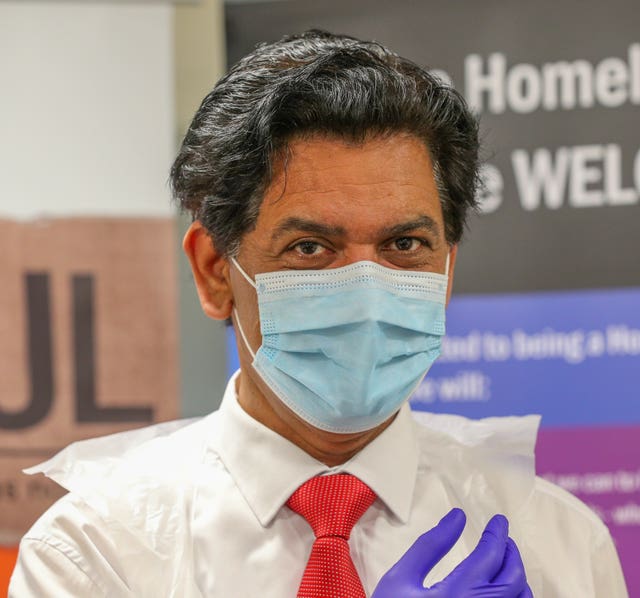
Zahid Chauhan, a GP in Oldham, observed:
On one side you’re trying to save patients and care for patients, and on the other side you’re trying to set up new systems. Third side (is) trying to educate your colleagues – clinicians and non-clinicians – to work using technology, fourth side you’re trying to educate patients to seek help in a different way.
Then among all those things you also have a personal life, family, children – think about them, think about how it’s impacting on them – and somehow build up your own resilience and your own coping mechanism as well.”
GPs have also seen an increased workload, in part taking on some of the work that hospitals are too overrun to do, and also dealing with the fallout of the pandemic and lockdown, including a rise in mental health issues.
“We haven’t got capacity”
That means some patients with less urgent health issues are sometimes struggling to speak to a doctor, which can lead to frustration.
Emily Ball, a GP in north-west England and an EveryDoctor team member, said:
They (less urgent patients) do need help but we haven’t got the capacity to give them that.
So we’re struggling and we’re trying to get through as much as we can every day, and our staff get a huge amount of abuse on the phone… people are really rude to our staff, really quite abusive.
It’s taking its toll on everyone in a variety of ways and I think people are losing the capacity to be kind to each other – and I think because we see people at their worst, when they’re at their most desperate, we cop quite a lot of it.”
But Ball cited an increased sense of unity between primary and secondary healthcare professionals as one of the positives to come from the pandemic.
And Morrell said she was “super proud” of the work she and her NHS colleagues had done.
“Honestly after these last 11 months I’ve never felt so close to my colleagues,” she said.
I feel very lucky – I don’t want that to sounds contrived because it’s such an awful time – but it has brought out the very, very best in the NHS for sure.
Story and image via Press Association