Thousands of doctors and nurses are concerned about inadequate supplies of personal protection equipment (PPE) amid fears some hospitals could run out entirely this weekend.
A British Medical Association (BMA) survey of more than 6,000 doctors across the country said a significant amount of them remain without the protection they need to guard against coronavirus (COVID-19).
Meanwhile, a Royal College of Nursing (RCN) survey of 14,000 nurses found that half of nurses have felt pressure to work without appropriate PPE during the crisis.
“Unprotected” and “exposed”
The survey results came after it was revealed that doctors and nurses in England will be asked to work without full-length gowns. They’ll also be asked to reuse items when treating coronavirus patients ahead of expected PPE shortages. The news has prompted outrage from unions.
BMA council chairman Dr Chaand Nagpaul said:
Two months into the Covid-19 crisis in Britain, we shouldn’t still be hearing that doctors feel unprotected when they go to work.
The Government says that one billion items will soon have been shipped, and while there have been signs of improvement, our research clearly shows that equipment is not reaching all doctors working on the front line.
We heard this week that a hospital boss resorted to asking the BBC for contacts at a clothing brand in a bid to get hold of gowns, and just yesterday the Health and Social Care Secretary said he could not guarantee that hospitals would not run out this weekend.
Meanwhile, the BMA has been inundated with approaches from companies offering to do their bit to supply the NHS.
This is a truly sorry state of affairs, and we renew our call for the Government to work with manufacturers to ramp up domestic supply.
Meanwhile, the Royal College of Nurses (RCN) has called on the government to take “immediate action” regarding the PPE situation. Nearly 14,000 nurses midwives and nursing support workers responded to RCN’s survey.
Donna Kinnair, chief executive and general secretary of the RCN, said:
This crisis is taking the lives of nursing staff, and their colleagues feel they’ve been left exposed.
All decision makers involved here need to get an urgent grip on the situation.
Nursing staff just want to do their jobs – they must be given protection in order to do so.
Giving evidence to the Health and Social Care select committee on 17 April, Kinnair told MPs:
As of this moment I am very worried that we don’t have enough PPE for staff to protect themselves, let alone facilitate giving it to relatives to be able to see their loved ones during the end of life care.
The BMA survey
The BMA survey found just under a third of doctors working in high risk, i.e. aerosol-general procedure (AGP) areas, and other non-AGP hospital settings said they were sometimes pressured to work without adequate protection. While 50% of doctors working in AGP areas said there were shortages, or no supply at all, of long-sleeved disposable gowns and disposable goggles. 56% said the same regarding full-face visors.
52% of doctors said scrubs and eye protections were in short supply, or not available, in other hospital settings.
Nagpaul added:
Too many doctors and healthcare staff have already lost their lives. We cannot afford to risk losing any more.
The BMA said one doctor surveyed said that current levels of PPE left them feeling as though they were being “thrown to the wolves”. Another said they shouldn’t be forced to choose between doing their job or keeping themselves and their family safe.
The RCN survey
Nearly 14,000 nurses, midwives and nursing support workers responded to the survey by RCN over the Easter bank holiday weekend.
Demands to get such equipment to NHS staff have intensified during the pandemic, as the number of healthcare professionals who have died after contracting coronavirus continues to rise.
A reminder of what we are demanding from the government since the #COVID19 outbreak began. We are here to fight your corner. pic.twitter.com/0T5dREJepG
— The RCN (@theRCN) April 16, 2020
The survey found that half of all respondents have felt pressure to care for a patient without the protection outlined in the current PPE guidance. One in ten (12%) nurses reported relying on face or eye protection that was homemade or that they’d bought themselves. And only 54% believed they have an adequate supply of alcohol hand gel.
Respondents include those working in high-risk environments, such as where patients suspected of contracting coronavirus are being treated on ventilators.
The RCN said that of those working in high-risk areas, 51% reported being asked to re-use PPE items that were marked as “single use” by manufacturers. Of those treating coronavirus patients elsewhere, 39% said this was the case.
The RCN has previously urged its members to refuse to treat patients as a “last resort” if adequate PPE isn’t provided. It said the results of the survey, conducted between 10 to 13 April, will be be shared directly with associated government agencies and regulators, including the Health and Safety Executive.
Government response
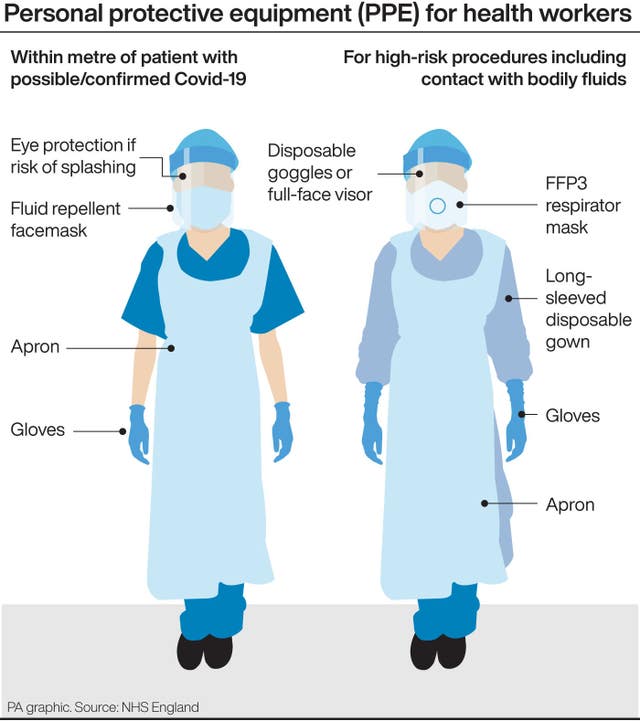
Public Health England (PHE) reversed its guidance on Friday evening which stipulated long-sleeved disposable fluid repellent gowns should be worn when treating coronavirus patients.
If the gowns aren’t available, clinical staff are now advised to wear “disposable, non-fluid repellent gowns or coveralls” or “washable surgical gowns”, with aprons, and to wash their forearms afterwards.
The updated guidance states that the “reuse of PPE should be implemented until confirmation of adequate re-supply is in place”, and that “some compromise is needed to optimise the supply of PPE in times of extreme shortages”.
A Department of Health spokesman said:
New clinical advice has been issued today to make sure that if there are shortages in one area, frontline staff know what PPE to wear instead to minimise risk.
On 17 April, Health Secretary Matt Hancock told a Commons committee that he would “love to be able to wave a magic wand” to increase PPE supplies.
At least 50 NHS workers have now died after contracting coronavirus.
















