Ambulance response times and A&E performance in England have dropped to their lowest levels on record while the backlog of patients waiting for care has continued to grow, new figures show. The latest data from NHS England shows the number of people in England waiting to start routine hospital treatment rose to a new record of 6.2 million at the end of February.
This is up from 6.1 million in January and is the highest number since records began in August 2007. But the figures also show that while the overall waiting list has continued to grow, the number of people waiting more than a year and two years have both fallen.

“Unacceptable levels”
Meanwhile, the average response time last month for ambulances in England dealing with the most urgent incidents – defined as calls from people with life-threatening illnesses or injuries – was nine minutes and 35 seconds. This is up from eight minutes and 51 seconds in February and is the longest average since current records began in August 2017.
Danielle Jefferies, analyst at The King’s Fund, said the latest figures show pressures are now reaching “unacceptable levels” in all parts of the health and care system. She added:
A&E departments remain full of patients in need of urgent care, and separate data shows a similar story in general practice and social care.
In March, 22,500 people waited over 12 hours to be admitted to hospital from A&E – a more than thirty-fold increase compared to a year ago.
Today’s data also shows ambulance service response times for serious health conditions are falling far below the national standards, with patients waiting over an hour for an emergency ambulance.
The NHS England figures also show ambulances in England took an average of one hour, one minute and three seconds last month to respond to emergency calls, such as burns, epilepsy and strokes. This is up from 42 minutes and seven seconds in February and is the longest time on record for this category of call-outs.
Urgent calls
Response times for urgent calls – such as late stages of labour, non-severe burns and diabetes – averaged three hours, 28 minutes and 13 seconds, up from two hours, 16 minutes and 13 seconds in February and another record. The latest A&E figures show that a record 22,506 people had to wait more than 12 hours in emergency departments in England in March from a decision to admit to actually being admitted.
The figure is up from 16,404 in February, and is the highest for any calendar month in records going back to August 2010. A total of 136,297 people waited at least four hours from the decision to admit to admission in March, another all-time high.
Just 71.6% of patients in England were seen within four hours at A&Es last month, the lowest percentage in records going back to November 2010. The operational standard is at least 95% of patients attending A&E should be admitted, transferred or discharged within four hours, but this has not been met nationally since 2015. NHS England said emergency departments are under significant pressure, with 2.17 million people attending A&E in March, a rise of nearly 20% month-to-month and the highest March ever.
“Emergency care is under particular strain”
Chris Hopson, chief executive of NHS Providers, told BBC Radio 4’s Today programme on Thursday morning that there are 20,000 medically-fit patients who cannot be discharged due to pressures on social care.
In a statement, he added:
Emergency care is under particular strain, with record levels of demand: record A&E attendances for the month of March and record ambulance call volumes from December to March.
We’re also seeing very concerning increases in ambulance response times and in the number of people waiting more than 12 hours in A&E before admission.
Trust leaders are deeply aware of the obvious risks to patient safety here and are doing all they can to manage these risks.
Trusts are also grappling with the ongoing impact of Covid-19. That’s meant more patients with Covid-19 in hospital beds, more staff off work with Covid-19, and more delayed discharges than anyone was expecting or had predicted.
Hugh Alderwick, director of policy at the Health Foundation, said the figures should be a “wake-up call” for Government. He added:
Part of the pressures are clearly due to Covid-19, with many staff off sick or self-isolating and the virus continuing to disrupt care.
Government must be honest about the impact of ‘living with Covid’ on the NHS and social care. But the health system was already struggling before the pandemic – hampered by a decade of underinvestment in health and social care and chronic staff shortages.
Staff and patients know that action is needed to address systemic workforce shortages – and today’s figures should be a wake-up call for Government.
Tackling the enormous backlog of unmet need depends on having enough staff to deliver care.
A fully-funded workforce plan for the NHS is urgently needed and must be a priority for Government.
Waiting more than two years
NHS England said that despite record volumes of 999 calls and ambulance call-outs for life-threatening conditions over the winter period of December to March, the service had managed to cut the numbers waiting the longest for hospital treatments.
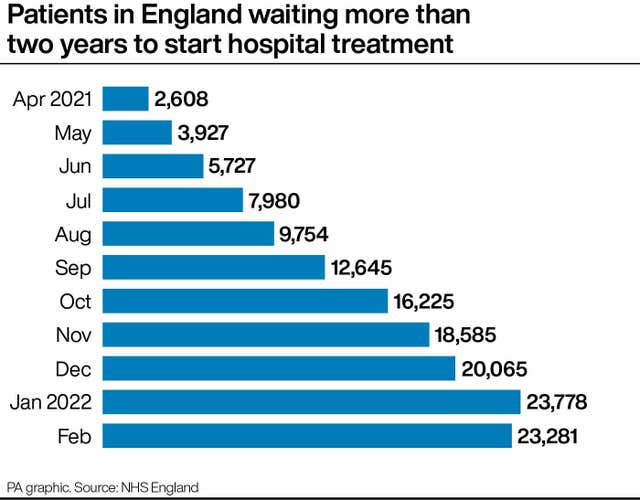
A total of 23,281 people in England were waiting more than two years to start routine hospital treatment at the end of February, down slightly from 23,778 at the end of January. But it is around nine times the 2,608 people who were waiting longer than two years in April 2021. The number of people having to wait more than a year to start hospital treatment also fell from 311,528 in January to 299,478 in February.
The NHS elective recovery plan sets the ambitions of eliminating all waits of more than two years, except when it is the patient’s choice, by July and all waits of more than a year by March 2025. The new backlog figures come after data obtained by the PA news agency showed dozens of NHS patients have waited more than three years for hospital care in England.
The figures, obtained through freedom of information requests, show at least eight people have been on the NHS waiting list for over four years, with one of these waiting for four-and-a-half years. NHS England national medical director Professor Stephen Powis said:
Nobody should be under any illusion about how tough a job NHS staff have on their hands, balancing competing priorities and maintaining high quality patient care.
Despite pressure on various fronts and the busiest winter ever for the NHS, long waits fell as staff continue to tackle two-year waits by July thanks to the innovative approaches to care they are now adopting – from same day hip replacements to dedicated mobile hubs for operations.
As ever, if you need help, especially over the often busy bank holiday weekend, please do come forward for the care you need through NHS 111 online and if it’s an emergency, dial 999 or go to your nearest A&E.
Featured image via – Flickr – Garry Knight
















